Patella Instability
What is Recurrent Patella Instability?
The patella (kneecap) is a small bone that shields your knee joint. It is found in front of your knee, in a groove called the trochlear groove that sits at the junction of the femur (thighbone) and tibia (shinbone).
Articular cartilage present below the patella and end of the femur cushion help the bones glide smoothly over each other when the legs move.
This joint is stabilised and supported by a network of soft tissues.
The Medial PatelloFemoral Ligament (MPFL) , shown above in orange and green , connects the inner side of the patella to the femur and helps to keep the patellar from slipping away from the knee. Damage to the MPFL leads to patella instability.
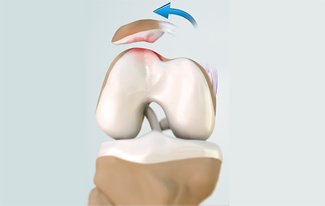
Patella instability occurs when the kneecap slides out of the trochlea.
The term “patella instability’ may indicate either a dislocation, where the kneecap comes completely out of its normal position, or a subluxation, where the kneecap only partially moves out and then goes back into its normal position as shown below..
Up to 80 percent of patients who have a high energy patella instability episode will have damage to the joint lining of the patellofemoral joint.
Greater than 90 percent of patients who have recurrent dislocations will have damage to the joint lining of the patellofemoral joint.
When dislocation of the patella occurs on more than one occasion, it is referred to as recurrent patellar dislocation.
The risk of further dislocation increases to almost 70% to 80% after two episodes of dislocation.
Causes of Recurrent Patella Dislocation
There are various causes of recurrent patella dislocation. Some of them include:
- Certain inherited traits:
- Kneecap that is seated too high in the groove
- Shallow trochlear groove
- Tight lateral patellar retinaculum and ligaments
- Valgus leg alignment (knock-kneed legs)
- Tibio-femoral rotational malalignment
- Trauma (twisting, bending, etc.)
- Skeletal immaturity
- Each dislocation causes stretching of soft tissues and increases the chances of recurrence and damage to the articular cartilage of the knee
Patellar dislocations are categorized as either low-energy or high-energy injuries.
In a low-energy injury, only a small amount of force is required to dislocate the patella, such as a sudden twisting injury in a knee with abnormally lax medial patellar ligaments and a dysplasic (flat) trochlea. Anatomic abnormalities that predispose a patient to a dislocation are a frequent finding in low-energy injuries.
On the other hand, a high-energy injury involves much greater force (usually in a knee with normal anatomy), such as that incurred by a direct blow to the patella during a sports activity.
It is important to distinguish between low and high-energy dislocation injuries because the expected outcome, extent of damage sustained in the knee joint, and treatment recommendations are different.
Symptoms of Recurrent Patella Dislocation
The common symptoms of recurrent patella dislocation are:
- Pain in the knee and around the kneecap
- Swelling
- Knee instability
- Feeling like it may dislocate again
Diagnosis of Recurrent Patella Dislocation
The dislocation of the patella can be diagnosed with a physical examination while you are sitting, lying down (supine, prone, and on your side), standing and walking.
Your doctor may order X-ray and advanced imaging with specific CT alignment scans to get a clear picture of the location of injury. You will also be advised to get an MRI done to assess the articular cartilage and other soft tissues of the knee.
Treatment of Recurrent Patella Dislocation
Recurrent patella dislocation can be treated by non-surgical or surgical methods based on the severity of the condition.
Non-surgical treatment
You may be recommended conservative treatment if your kneecap has dislocated only once or twice. You may be recommended a limited period of immobilisation with a brace, cast or splint. Your physiotherapist may also attempt to stretch the structures on the outside of the knee and suggest certain exercises to strengthen your muscles. Analgesics and non-steroidal anti-inflammatory drugs may be prescribed to relieve pain and swelling.
Surgical treatment
Surgery is recommended when non-surgical treatment is found to be ineffective in relieving the symptoms of recurrent patella dislocation.
The goals of surgery are to correct any malalignment issues, balance soft tissues, and reconstruct torn or deficient ligaments (especially the MPFL). Many different types of operations have been described in the medical literature for extensor mechanism malalignment. The decision of which procedure to perform is based on the number and extent of anatomic problems that exist.
This is where the physical examination and either CT or MRI determine important factors such as the lower limb rotational alignment (femoral anteversion and external tibial torsion), shape of the trochlear groove, the tibial tubercle-trochlear groove (TT-TG) distance and the patellar height.
There are two broad types of surgical patellofemoral joint stabilisation procedures, called
- Proximal stabilisation by MPFL Reconstruction and Lateral Retinacula lengthening
- Distal realignment by Tibial Tubercle Osteotomy .
Advance imaging organised by Dr Berton will have determined if there is a boney malalignment is present predisposing the patient to Patella instability which may require distal realignment or whether the problem is primarily a soft tissue problem.
MPFL Reconstruction
All procedures performed to treat the dislocation will first involve arthroscopy.
Arthroscopy is a minimally invasive procedure that. The injured joint surface called articular cartilage can be smoothed to remove any loosely attached articular cartilage fragments.
To reconstruct the torn medial patellofemoral ligament, holes are then drilled in the patella and femur, and a piece of hamstring tendon (tissue connecting muscle at the back of the thigh to the knee) is passed into the holes to replace the torn MPFL. The tendons are fitted into place with the help of screws and anchors as shown .
Distal Realignment by Tibial Tubercle Osteotomy.
An Osteotomy is a surgical procedure where a bone is cut and repositioned to alter alignment of soft tissues or a joint.
Above is an example of 3D CT showing increased lateralization of tibial tubercle predisposing to patella instability which responded to tibial tubercle anteromedialisation by Fulkerson Osteotomy shown below.
Screws are used to hold position of the tuberosity after osteotomy until complete healing takes place .
Postoperative Care after Recurrent Patella Dislocation Surgery
As a post-operative management procedure, you will be advised to use crutches and wear a brace usually for 6 weeks. Once the soft tissues and or osteotomy has healed activities can be increased.
A physiotherapist will have met you before surgery and will supervise a rehabilitation individualised plan .
Recovery is lengthy with MPFL reconstruction requiring avoidance of at risk activity in the first 3 months from surgery.
Recovery from Tibial tubercle Osteotomy is more complex and lengthier than MPFL reconstruction with risk of tibial fracture in the first 6-12 months after surgery.